Investigators at Weill Cornell Medicine and NewYork-Presbyterian have used advanced technology and analytics to map, at single-cell resolution, the cellular landscape of diseased lung tissue in severe COVID-19 and other infectious lung diseases. In the study, published in the May 2021 issue of Nature, the researchers imaged autopsied lung tissue in a way that simultaneously highlighted dozens of molecular markers on cells. Analyzing these data using novel analytical tools revealed new insights into the causes of damage in these lung illnesses and a rich data resource for further research.
“COVID-19 is a complex disease, and we still don’t understand exactly what it does to a lot of organs, but with this study we were able to develop a much clearer understanding of its effects on the lungs,” says co-senior author Olivier Elemento, PhD, Director of the Englander Institute for Precision Medicine, Associate Director of the Institute for Computational Medicine, Director of the Laboratory of Cancer Systems Biology at Weill Cornell Medicine, and Co-Director of the WorldQuant Initiative for Quantitative Prediction, which funded the technology for single cell analysis of tissue. “I think the technological approach we used here is going to become standard for studying such diseases.”
Traditional tissue analysis, often using chemical stains or tagged antibodies that label different molecules on cells, can reveal important features of autopsied tissues. However, this approach is limited in the number of features it can mark simultaneously and usually doesn’t allow detailed analyses of individual cells in tissues while retaining information about where the cells were in the tissue.
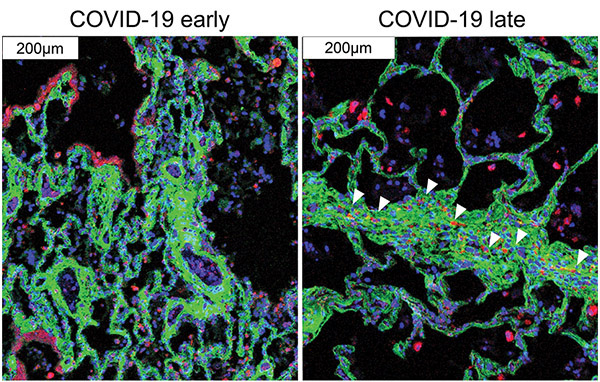
The Weill Cornell investigators employed imaging mass cytometry, a technology that largely overcomes those limitations by using a collection of metal-tagged antibodies that can simultaneously label up to several dozen molecular markers on cells within tissues. A laser scans the labeled tissue sections, vaporizing the metal tags, and the metals’ distinct signatures are detected and correlated with the laser position. The technique essentially maps precisely where cells are in the sample as well as each cell’s surface receptors and other important identifying markers. Altogether over 650,000 cells were analyzed.
The researchers applied the technique to 19 lung tissue samples autopsied from patients who had died of severe COVID-19, acute bacterial pneumonia, or bacterial or influenza-related acute respiratory distress syndrome, along with four lung tissue samples autopsied from individuals with no lung disease.
The findings in samples from COVID-19 cases were broadly consistent with what is known about the disease but clarified this knowledge in much finer detail. They showed, for example, that alveolar epithelial cells are the main targets of infection by SARS-CoV-2. The analysis suggested that these infected cells are not solely singled out for attack by lung-infiltrating immune cells, which may help explain why inflammation often keeps worsening in severe COVID-19 and ends up causing such extensive and relatively indiscriminate damage.
Age and sex, two major factors in mortality risk for COVID-19, made no apparent difference at the histologic level once COVID-19 had progressed to the severe stage.
The results also showed that macrophages are much more abundant in the lungs of severe COVID-19 patients compared to other lung diseases, whereas neutrophils are most prevalent in bacterial pneumonia, a distinction that may be relevant to the development of future treatments for these infectious diseases.